October 23rd, 2023: Seneca Tien Pham is here!
It’s one of the happiest moments of my life. Our second daughter with my wife Marissa is born with zero complications at St. Joseph’s birthing center in Reading, PA. It was magically uncomplicated and in the back of my mind I held a weird shoe drop moment. Not knowing what that could be, I just enjoyed Seneca’s presence as much as I could by taking some PTO for the week away from work. My wife came through pregnancy without issue and our first daughter, now 6-year-old Isadora, was delighted to be a big sister. What could go wrong?
Out of work tracker: 1 week





October 29th, 2023: The Other Shoe.
Just under a week after Seneca was born, I was hospitalized for a week at Chester County Hospital for extreme edema, severe hypertension, and unregulated diabetes. The other shoe dropped on me, and it was not forgiving. As I went through multiple tests and procedures, it was discovered that my kidneys are no longer functioning as they should. At first, they thought it was just an acute issue, but post biopsy of my left kidney the doctors found irreversible scaring of my kidneys and sadly they are at end-stage failure. Doctors then inserted a subclavian catheter in my jugular so I can begin hemodialysis to start what my kidneys could no longer do: filter out my blood. Because dialysis is only life-sustaining, the search for organ donation and subsequent kidney transplant is the best option to normalize and extend my life.

November 3rd, 2023: Out of the Hospital
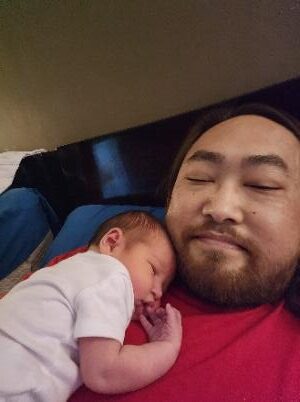
I was deemed ready for discharge on Friday, but the bad news is already given. I have to put my body through hemodialysis 3 times a week for 5 hours each session at an outpatient center to accomplish what my kidneys cannot. Each session is exhaustive, but I was fighting through because it was making me feel better. Each session brought on new life. I was finally able to hold our baby Seneca and that was all I needed to know that I was getting better. Thank you to all the nurses and techs at Fresenius Kidney Care in West Chester. You have provided unwavering support in my journey of renal failure and your skills in making hemodialysis as painless is possible is always appreciated.
Out of work tracker: 2 weeks
November 13th, 2023: Unregulated Diabetes
I know I must hit the source of my problems as the kidney failure is deemed to be from diabetic neuropathy. Basically, the high blood sugar made the kidneys work in overtime and, over a decade, they finally decided to break down. I get to an endocrinologist asap and I start on insulin (both fast-acting and long-acting). Diabetic medication, pill wise, is very renal adverse. Yes, the oral diabetic medication that I was taking exacerbated my kidney disfunction and most likely advanced the kidney failure. I was also overusing NSAIDs, as both a diuretic and a sleeping aid. Those also help in kicking my kidneys to the curb. If your kidneys are okay, you can take NSAID’s periodically, but I suggest never taking it for months. If you need a sleeping agent, please use melatonin. If you need something stronger, please investigate Benadryl, the sleeping agent in most PM medications. No need for the other adulterants if you don’t need them.
Out of work tracker: 3 weeks
December 6th, 2023: Severe Hypertension
While first hospitalized in October into November, I received a team of cardiologists, headed by Dr. Jan, that want to ensure there wasn’t anything wrong with my heart. Many blood tests and a stress test are prescribed to see what’s going on. My blood pressure was through the roof when I was first hospitalized. The doctors were concerned I could have a heart attack or a stroke at any time. Luckily my blood pressure, although still a bit high, calmed down after several hemodialysis sessions.
At this early December follow-up I go through a stress test where they inject radioactive fluid and track it around your heart with imaging (EKG) and get the heart activity to 70%. It turns out there is something up with my heart, the stress results were positive, and a PA told me to ‘start taking baby aspirin and someone will be in touch for a follow up’.
Out of work tracker: 6 weeks
December 13th, 2024: Kidney Transplant List
My wife, our newborn daughter Seneca, and I travel to center city Philadelphia to meet with Dr. Singh of the Nicoletti Kidney Transplant Center at the Jefferson Transplant Institute. She is a brilliant doctor that understands the transplant process inside and out. She guides us from the beginning in what we need to do to setup the transplant process. She tells us that there could be the possibility of receiving both a pancreas and kidney transplant and possibly curing both my diabetes and kidney failure at the same time. Here’s to wishing. Dr. Singh lists a colonoscopy, a CT scan, and cardiac review as some of the last remaining screenings I must do to get on a transplant list. She set us up with a team and a task list of what is needed to move forward.
Out of work tracker: 8 weeks
January 8th and 9th, 2024: Peritoneal Dialysis
Hemodialysis, although very effective, is quite exhaustive and time and travel are needed to be there at an outpatient location. This hinders my ability to return to work and provide for my family. I choose to go down the path of peritoneal dialysis so that I can run the dialysis at home while I sleep. I met with Dr. Tan of Jefferson Health on the 8th to screen and schedule me for Peritoneal Dialysis tube insertion. January 9th was my birthday. As I turned 48, my birthday gift to my self was returning to Jefferson for a CT scan to ensure that my body would be ready for a kidney transplant. Now I just need the colonoscopy to be cleared for getting on that transplant list, either from a living donor or deceased (what is a 9 year waitlist).
January 16th, 2024: Peritoneal Tube Implant
Dr. Tan is no nonsense and knows the urgency that my life depends on these procedures. She advances my Peritoneal implant surgery for 1/16/24 and my family takes me into Philly for the procedure. We were greeted with a winter snowstorm. The operation went without issue, but it feels like someone shot you in the gut post recovery. I do not wish dialysis treatment on any human. Either way you go, it’s a fight and exhaustive. Don’t let your kidneys go past the point of functionality as there is no turning back or healing of these organs.
Out of work tracker: 13 weeks
February 2nd, 2024: The Start of PD
Peritoneal Dialysis (PD) starts after 2 weeks of PD training while still doing hemodialysis at Fresenius, I was ready to do dialysis on my own at home. Majority of the PD is infection prevention: making sure you are working from sterile equipment and keeping clean. The other thing you need you be aware of is the huge amount of supplies stored for PD and the incredible amount of waste that is produced to keep sterile. I start setup around 8:30pm and sterilize all work surfaces and equipment, keep the door closed and family and pets out, and connect the dextrose fluid bags to the equipment and into my PD catheter, a direct line into my stomach, and with many feet of drainage tubes connected to the toilet for waste output. Most of the time overnight treatment takes me till about 7:30am to disconnect safely and be done with PD for the day. That’s 11 hours a day, every day. Hopefully I can intertwine treatment during sleep, and it won’t seem so bad.
Out of work tracker: 15 weeks
February 12th and 13th, 2024: Colonoscopy/Endoscopy
The dreaded colonoscopy is here. Prep day is an abysmal day. They literally want everything out of your digestive track, and they make you take many laxatives to ensure that is true. Now add nightly PD process to the prep and realize how difficult it is to deal with the prep laxatives and to be connected, sterilely, to PD equipment and having your abdomen to be filled, dwelled, and drained throughout the night. I could have not gone through this without my wife’s assistance, in fact she has been by my side ever since I was first hospitalized, organizing all medical appointments and advocating for efficiency in my care. I cannot thank her enough for being my support structure.
The actual procedure was uneventful, excluding a second winter storm that greeted my family yet again in route to the hospital, but they did find one polyp that was removed immediately. Both Endo and Colon show no issue and they want to do this in another 7 years. Finally, some good news. My wife, who has been in constant contact with the kidney transplant team, informs them that I should now have completed the last test for getting on the kidney transplant list. Oddly we get a call from the team at Jefferson, saying that there is an issue with my heart stress test from back in December, and we should schedule a follow up with the cardiologist asap. If it were not for transplant…
Out of work tracker: 17 weeks
February 20th & March 7th, 2024: Another Shoe?
We advocate for a follow-up with the cardiologists and get the next business day appointment on February 20th. The heart stress test had occurred on Dec 6th but I was not scheduled for a follow-up. At this new consult, it’s informed to me that they are surprised I’m not complaining about any heart issues and that there was significant shadowing to my heart that is of major concern. They want to schedule a heart catheter to go up a radial artery with a camera and poke around, perhaps doing an angioplasty if any blockage is found. That was scheduled for March 7th and the results were shocking. 5 of my main coronary arteries are blocked with the primary 3 being 98, 96, and 86 percent blocked. Angioplasty will not be sufficient, and Dr. Jan recommends quintuple open heart bypass surgery.
I’m devastated.
I have forgotten about the hypertension issues and now I’m faced with major surgery with the alternative being a heart attack and/or stroke. I’m referred to Dr. McCarty, a cardiothoracic surgeon, for the bypass consultation and operation. We meet with her rapidly and she’s noncommittal on the number of bypasses she expects to perform. She says she won’t know till she’s in the operation but does know that it will be at least a triple bypass. Dr. McCarty sets March 14th for the surgery, a mere one week later. For the first time, I’m truly concerned for my future. Before I was okay mentally to take care of what I needed to get on the transplant list and to keep my survival going. Now I enter major surgery that could take me out in an instant if something goes wrong. I reach out to my brother Duy the evening before surgery and ask him to promise me that he will take care of my girls if I don’t make it. It was emotional, but he promised and says, ‘as if they were my own’. He also has two daughters, so he knows what to do in case things go wrong.
During all of this for the month of February I’m experiencing significant issues with at-home PD care where it’s not filtering as I need it to, and the dwelling of fluid in my abdominal for hours on end is preventing me from getting any sleep. I’m exhausted and my blood work is terrible. I have regressed. They move me back to hemodialysis for the time being. Hello Fresenius, my old friend.
Out of work tracker: 19 weeks
March 14th, 2024: Open Heart Bypass and Hemorrhaging
Operation day arrives. As it goes, Dr. McCarty could only bypass the first two arteries as the hemorrhaging became too much to safely continue. Hopefully bypassing the two main arteries is enough. It was a long operation as I find myself waking up in the Chester County Hospital ICU, tied down, with a breathing tube down my throat. I hear my wife’s voice. It’s reassuring knowing that I’m still alive and I squeeze her hand to let her know I’m coming out of it. It’s painful, my chest feels like 6 buses ran me over but in the back of my mind I realize I have made it through. I’m still here and I’m grateful for all the doctors and nurses that made it happen. I’ve been given many sedatives to keep me under. It’s a lot for any human to endure.
The hospital stay was stamina draining. I’ve been in this environment too much. Nurses come in and poke and prod you every 4 hours, you can’t get any sleep and the food is filling at best. My throat is sore from the breathing tube and chest is recovering slowly from my sternum being opened. I have drainage holes and tubes everywhere and it’s all incredibly frustrating. I keep focus that this will return my health and get me clearance to be on the kidney transplant list. It’s easy to forget with throbbing chest pains, but I hold strong.
Determined to be discharged, as I have already missed Isadora’s birthday on the 19th, I do what I can to have them clear me to go home. You want me to walk a lap around the ICU floor? Here’s two. Holding me back is bleeding from one of the 3 drainage holes at middle of my chest to clear my lungs. It was bleeding so much that they had to tap my left lung to drain a liter of fluid out. I could breathe so much easier post tap, but it also increased my cough force, and it feels like a knife cutting through my chest at each cough. They give you a “chest pillow” to help the pain, but the assistance is minor at most and sometimes cough comes when you don’t have the pillow readily available.
Out of work tracker: 20 weeks
March 22nd, 2024: Hospital ICU Discharge
I’m going home. Bleeding was stopped on the middle drainage hole using some silver nitrate. I miss my daughters terribly. Big thank you to my brother Duy, sister Oanh and family friend Val, who helped Marissa with Seneca so my wife could visit me regularly in my ICU room. Her and their presence was a great motivator and squashed the loneliness that comes with these recoveries. It’s been a week and a day and if you asked me if I could be discharged earlier in the week, I would easily tell you no. Progress happened slowly but day by day. Thank you to the entire Chester County Hospital ICU staff that got me to discharge possibilities. Their support and care were invaluable, and their encouragement was essential.
Out of work tracker: 21 weeks
March 29th, 2024: Mending at Home
It’s been a week since I’ve been home, and I’ve been slowly getting better. Chest pain is still excruciating, and my sleep schedule is still all jacked up. I get at most 2 hours of sleep at a time due to the hospital conditioning me that way. I sleep when I can, including during hemodialysis. Sleep feels like the only time my body can repair itself. I expect it to take me another week to get my sleep schedule normalized. I get home visits once a week each from a Physical Therapist, Occupational Therapist, and a visiting Home Nurse to ensure that I’m still progressing to cardiac normalcy and to keep me active. Sprinkle in three times weekly visits to Fresenius and you currently have my weekly plans.
Out of work tracker: 22 weeks
April 4th – 6th, 2024: The Slow Mend
Another week goes by in slow progression. I’m still on the “every 6 hours” of maximum strength Tylenol for pain management and my sleep schedule is slowly turning to normal. Hospitals really do a number on that. My wife, now chauffeur, drives me to follow-up visits with both my cardiologist and cardiac surgeon, who expect a minimum 3-month recovery for me (which means at least three months till I may finally be added to the transplant list). In the meantime, I just had a consultation for an arteriovenous fistula for hemodialysis in lieu of my subclavian catheter. The clavicle catheter was meant to be temporary, but the PD experiment was not successful, and I have had to rely on these tubes to filter my blood. Each use of the tubes essentially embedded in my neck pushes the possibility of an infection, so another catheter it is and another scheduled procedure for HD.
Hopefully we can kickstart the kidney donation match soon.
A new kidney would mean getting rid of all catheters in my body and the less holes, the better. There’s also an innovative procedure involving a combined kidney and blood stem cell transplant that will generate the living donor’s white blood cells in me allowing me to avoid the lifelong use of immunosuppressive drugs. The immunosuppressants I would otherwise take post-transplant have some nasty side effects. Additionally, the new white blood cell procedure could increase the long-term acceptance and potentially double the life span of a donated living kidney – something I’m very interested in as a relatively young man. A living donor organ may graciously provide 20-25 years of life. Alternatively, the waitlist for a deceased organ donation is up to nine years (while relying on regular dialysis), with such a donation sustaining me for as little as ten years before I would have to revert to dialysis again, as a later life subsequent transplant would be unlikely.
Another shoe? I should start a footlocker. So, Fresenius calls and states they’d like me to go to the emergency room. My hemoglobin is way low, and they’d like blood work done at the hospital and if the levels are the same, they’d like a blood transfusion asap. They don’t want me to randomly pass out and risk retraumatizing my sternum. I think it may be overkill but I will comply with what they are asking. It’s the only thing I can do.
Back home after 2.5 days at the Chester County Hospital. It’s confirmed, I do not enjoy hospital stays. I was pushed around the ER for several hours and finally got a room in the Progressive Care Unit at around 3am. “Hurry up and wait” should be the hospital’s motto. It’s not the people it’s the protocols. People are great and are only doing what they can to keep you healthy and/or alive. My stay was a lot of observations…nothing I couldn’t do at home. I had to push the doctors to let me be discharged today. Hemoglobin levels are still low, but that’s how I roll it seems. Doctors agreed and suggested staying the course with medication and dialysis will turn that number around.
Out of work tracker: 23 weeks
April 12th, 2024: Recovering Turns a Corner
I’ve finally turned a corner on my recovery from open-heart bypass surgery. The pain has subsided and I’m down to about a dose Tylenol every 12 hours instead of every 6. I can make my own breakfast and have full motion and can finally nap on my side. I’m still under surgery restrictions, so no holding Seneca yet, but I feel this objective closer than a week ago when the pain was too much to even think about holding my baby girl. I can walk to pick up Isadora from her bus drop-off from school. It’s little things that I’m progressing through that lets me know I’m headed in the right direction. Fresenius is keeping the water weight off me and I’m revolving around 154 to 160 lbs. throughout the week. It’s motivating that each day brings pain relief from the open-heart surgery. I can’t wait till it’s a scar instead of a sutured line.
Out of work tracker: 24 weeks
April 24th, 2024: Another Day, another procedure.
It’s AV fistula day. Fistula is a procedure that connects an artery to a vein in preparation for dialysis. My vascular surgeon Dr. Lee performed the procedure flawlessly. My left arm is in pain, something I’m getting used to, but the procedure was quick and I was awakened from the anesthesia after an hour of surgery. This is all to provide a new pathway for the dialysis connections and to replace the subclavian catheter. It may take 8 to 10 weeks for the fistula to be ready for dialysis, so I’ll be still using the subclavian catheter until that is ready. The fistula does put a hamper on holding Seneca with my left arm, but my right arm can still hug her and hold her for a minute or two. That’s something I’ve been missing ever since the open-heart surgery.
Out of work tracker: 26 weeks
May 2, 2024: Discharged from Home Nursing visits.
Today was the last day of the nurse home visits as well as the physical and occupational home visits. They deem me to be at a state that those visits are no longer necessary. So, there’s progress there, now I just need to get through cardiac physical therapy which will be started on May 20th. I don’t expect any issues as the majority of physical goals have been relatively easy for me to accomplish. I’m headstrong in getting better for me and my family. I was cleared to drive on April 23rd by my cardiac surgeon, Dr. McCarty. It feels good to be independent in that nature again and the seatbelt pressure on my scar no longer hurts, which makes it that much easier to drive. I drive myself to my dialysis sessions which I have changed to Tuesday, Thursday, and Saturdays in the anticipation of starting work again. It’s been a long time and I expect to be back in part time starting June 3rd. I’m excited to get back to some sort of normalcy and starting work again will be a big part of that.
Out of work tacker: 27 weeks
One response to “My Story”
-
I will keep you in my prayers . I worked in the credit dept at Singer and always remember how helpful you were.
Have faith and I’ll keep you in my prayers.
Leave a Reply